Do You Need a TPA?
Between navigating compliance regulations, processing claims, and designing cost-effective plans, employee benefits can feel overwhelming, especially as healthcare continues to evolve. That’s where third-party benefits administrators (TPAs) step in.

In This Article
Employee benefits are a key factor for any businesses, helping attract top talent, boost satisfaction, and drive engagement. Yet, managing benefits can be complex and time consuming, creating major challenges for businesses—which is why nearly 50% of employers still don’t offer them. Between navigating regulations, processing claims, and designing cost-effective plans it can all feel overwhelming, especially as healthcare continues to evolve.
That’s where third-party benefits administrators (TPAs) step in. They simplify the process by taking care of the busywork and allowing you to focus on growing your business. A TPA doesn’t just reduce the headaches of managing benefits—it makes offering them possible in the first place. Companies that work with TPAs often experience reduced healthcare costs, improved employee engagement, and greater operational efficiency. With alternative models and self-funded plans, businesses that previously thought they couldn’t afford to provide benefits can now compete with larger organizations.
But what exactly is a TPA, and do you really need one?
What is a TPA in healthcare?
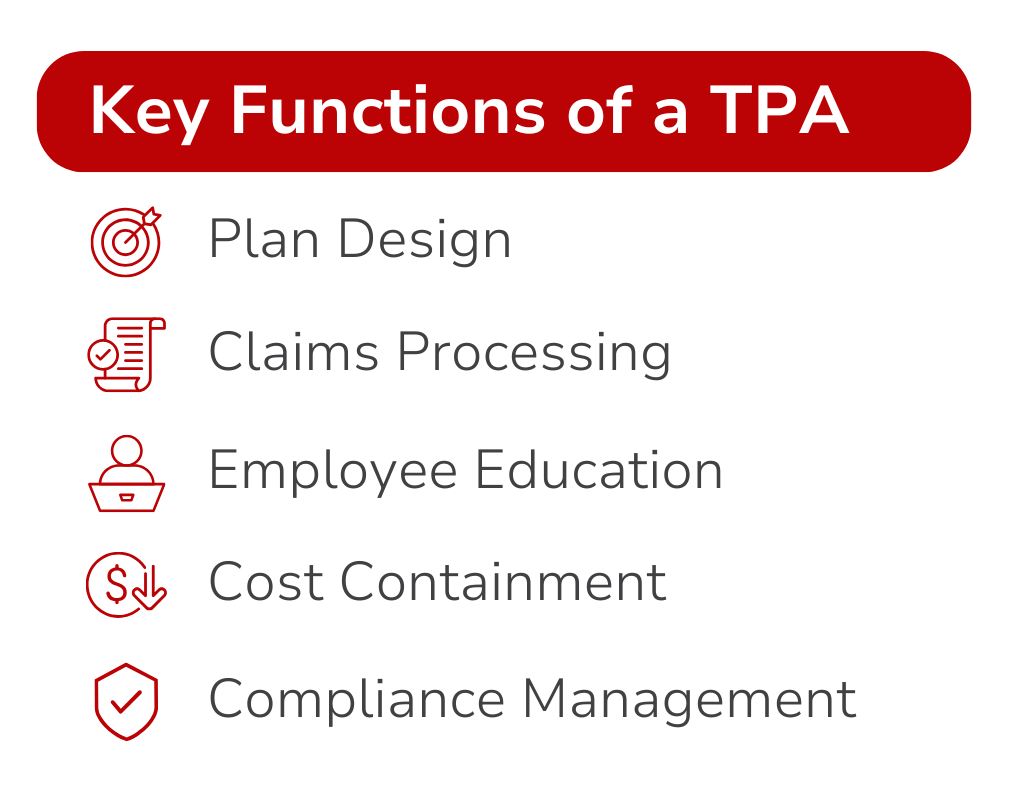
Like the name suggests, a third-party benefits administrator primarily handles the administrative side of employee benefits. That means taking responsibility for important tasks like claims processing, compliance management, and benefits plan design. Benefits administrators become the crucial link between employers, employees, and healthcare providers. Their role is indispensable in creating efficient, cost-effective benefits programs.
Claims Processing: involves handling the entire lifecycle of claims to ensure they are managed efficiently and accurately, which allows employees to access care without unnecessary and frustrating delays.
Compliance Management: involves helping businesses navigate complex healthcare laws to minimize the risk of penalties.
Benefits Plan Design: allows benefit administrators to work with businesses to create tailored plans that align with company goals, and possible budgetary constraints.
One of the primary distinctions between TPAs and insurance companies is their independence. Benefit administrators are not tied to a single provider or carrier, which means they have the flexibility to help businesses create customized plans. It’s important to note that a TPA is not an insurance carrier, and they do not directly provide coverage. Rather, a benefits administrator works with their clients to build and manage their healthcare benefits plans.
The growing need for benefits administrators
Managing employee benefits has become increasingly complex due to rising healthcare costs and ever-evolving regulations. For many businesses, particularly small and medium-sized companies, handling these challenges in-house is not practical. Benefits administrators provide the expertise, flexibility and affordability necessary to navigate this while offering significant advantages to employers by allowing them to build self-funded benefits plans.
Affordability
Providing benefits the conventional way is expensive, especially for small businesses. Insurance premiums continue to rise, making it harder for companies to even afford benefits let alone something that’s market competitive. Benefits administrators can help lower costs by working with self-funded plans and other cost-saving solutions that keep their claims fund as stable as possible. And when it comes to preparing for the unexpected, a TPA can enable an employer to manage the financial risk of offering a health plan by adding stop-loss coverage, which protects against high-cost claims.
Self-Funded Plans
Unlike fully-insured plans, which require purchasing health insurance from an insurance provider that then assumes the risk, self-funded plans allow businesses to take control of their benefits programs. The higher costs associated with fully insured plans can make them a less feasible—or less desirable—option, leading many employers to explore alternative approaches such as partnering with a TPA.
Flexible Plan Options
Traditional insurance options often come with set structures that just don’t work for every business. Benefits administrators allow employers to customize benefits by offering flexible options that don’t take the cookie-cutter approach. Employers can provide employees with more choices for their healthcare benefits which improves access to care and overall satisfaction.
This flexibility helps businesses avoid paying for coverage they don’t need while still offering benefits that their employees want.
Guidance from the Experts
Healthcare regulations and compliance requirements are constantly changing, making it difficult for businesses to stay up-to-date. This is where a TPA’s experience in managing benefits programs and ensuring compliance with complex federal regulations comes in handy. Instead of tackling these challenges alone, businesses can rely on their benefits administrator to manage those important details, reducing the constant administrative strain and lowering their risk of mistakes.
Without a TPA, businesses would be stuck with minimal options that are unaffordable and impossible to understand. By working with a TPA, businesses can take a more practical approach to benefits administration—offering self-funded plans, gaining expert guidance, customizing plan options, and keeping costs under control while still providing quality healthcare options for their valued employees.
How Planstin stands out as a TPA
At Planstin, we're not just another third-party administrator—we redefine what benefits administration can be. With a mix of user-friendly technology, personalized support, and flexible solutions, we make managing employee benefits simple and stress-free.
In-House Support & Technology
Our job is to make life easier for our clients and ensure their employees feel supported- whether it’s through our easy-to-use technology, 1:1 guidance, or our hands-on care coordination services. At Planstin, we provide these services at no extra cost for our clients, in addition to the flexibility, affordability, and expert guidance expected from a TPA. Plus, our in-house support, customized solutions, and wide range of benefit options ensures businesses, and their employees, get the care they need.
We know that managing employee benefits can be overwhelming. That’s why we offer more than just average administrative support. Unlike TPAs that simply process paperwork, we take a hands-on approach with benefit advocacy, streamlined enrollment, educational resources, and compliance support.
Planstin makes open enrollment and benefits management stress-free with our Enrollment Manager, a tool designed to simplify the process for employers, HR teams, and employees alike.
This user-friendly platform helps businesses stay organized and gives employees the clarity they need to make informed decisions about their healthcare. At the end of the day, our goal is to take the hassle out of benefits so businesses can focus on what they do best.

Benefits Solutions
Planstin specializes in creating benefits programs tailored to the needs of businesses rather than forcing them to fit into predetermined, one-size-fits-all insurance models. We offer the kinds of things you’d expect: dental, vision, comprehensive care. But we also offer the kinds of things you might not, such as Direct Primary Care (DPC) memberships and HealthShare memberships. This unique approach—combining traditional and nontraditional solutions, is what separates Planstin from other TPAs.
Preventive care and wellness are also key components of what we offer. We can help your employees gain access to mental health resources, wellness management and other tools that support long-term health and well-being. With simplified processes and personalized care coordination, employees can feel confident navigating their benefits.
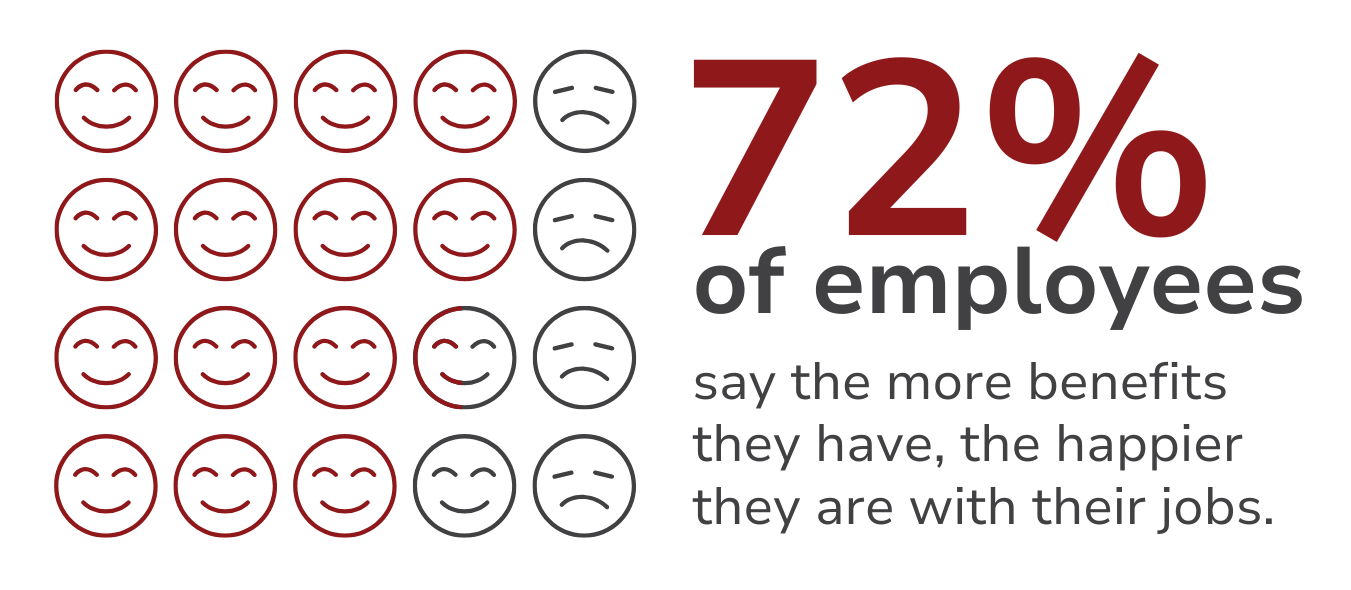
The employee advantage
A great benefits program isn’t just about checking a box, it’s about making life easier for employers and employees. Depending on the TPA, they can provide significant value to employees, transforming the employee experience by offering benefits that actually work for them. When employees have the freedom to choose their healthcare providers and customize their benefits options they feel more in control of their healthcare decisions.
When you partner with a TPA it tells your employees that you take their benefits plan seriously. Showing your employees that you care can win you favor with your team and boost morale. When employees feel supported and valued, it leads to increased productivity and a more engaged workforce. A win for everyone. Employees also benefit from better access to care, education resources, and a sense of security knowing their healthcare needs are covered. These advantages translate into a healthier, happier workforce and contribute to the overall success of the business.
“I highly recommend considering Planstin Administration as a way of approaching healthcare benefits for a wide range of coverage needs, with minimal out-of-pocket costs for your employees and business budget.”
Ashlee Hogancamp - Founder, Herban Market
Beyond benefits: The right TPA makes all the difference
There’s no denying that employee benefits are necessary for attracting and retaining top talent. As businesses try to accomplish this, the need for benefits administrators continues to grow. Unfortunately, not all TPAs are created equal, and finding the right one might seem overwhelming. Fortunately, you’ve found your way to this blog, and Planstin’s Administration.
While most TPAs provide guidance, flexibility, and affordability, Planstin goes beyond just handling the basics and takes a hands-on approach in empowering clients with adaptable options, dedicated support services, and easy-to-use technology. We also understand that a truly great benefits administration partner helps businesses take care of their employees while keeping costs under control, creating a win for both employers and their teams. At the end of the day, we’re here to make your life easier and help you succeed—like a trusted TPA should.
With the right TPA by your side, offering benefits is within your reach.
Book a free meeting with one of our Benefit Guides to learn how you can make benefits available to your team.
Explore
SUGGESTED FOR YOU


I WANT TO...
LOGIN
CLAIM INFORMATION
Payer ID: 65241
Planstin Administration
P.O. Box 21747
Eagan, MN 55121
© 2025 Planstin Administration - All Rights Reserved


