ACA 2025 Update: Reporting and Penalty Adjustments
The IRS decision to lower employer shared responsibility penalties in 2025 is a rare move. However, it comes alongside increased penalties for missed reporting deadlines. Take this opportunity to optimize your benefits strategy and make sure you are avoiding the penalties altogether.

In This Article
Since the Affordable Care Act passed, the Section 4980H penalty amounts have been steadily rising, going from $2,080 in 2015 to $2,970 in 2024. However, in late 2024, the IRS did something unexpected: for the first time ever, they lowered the ACA’s Employer Shared Responsibility Payment (ESRP) penalties.
The choice to decrease the larger penalty amounts for the 2025 tax year is surprising and should not be taken as an indication that these penalties will continue to be reduced. In fact, along with this decrease in the larger penalty amounts, the IRS has increased some of the reporting penalties—effective for those reporting for the 2024 tax year.
A quick ESRP (Section 4980H) penalty refresher
If your company has 50 or more full-time (or full-time equivalent) employees, the ACA requires you to offer affordable, minimum-value health coverage to your full-time employees and their dependents. If you don’t there are two potential penalties, of which you will pay one or the other.
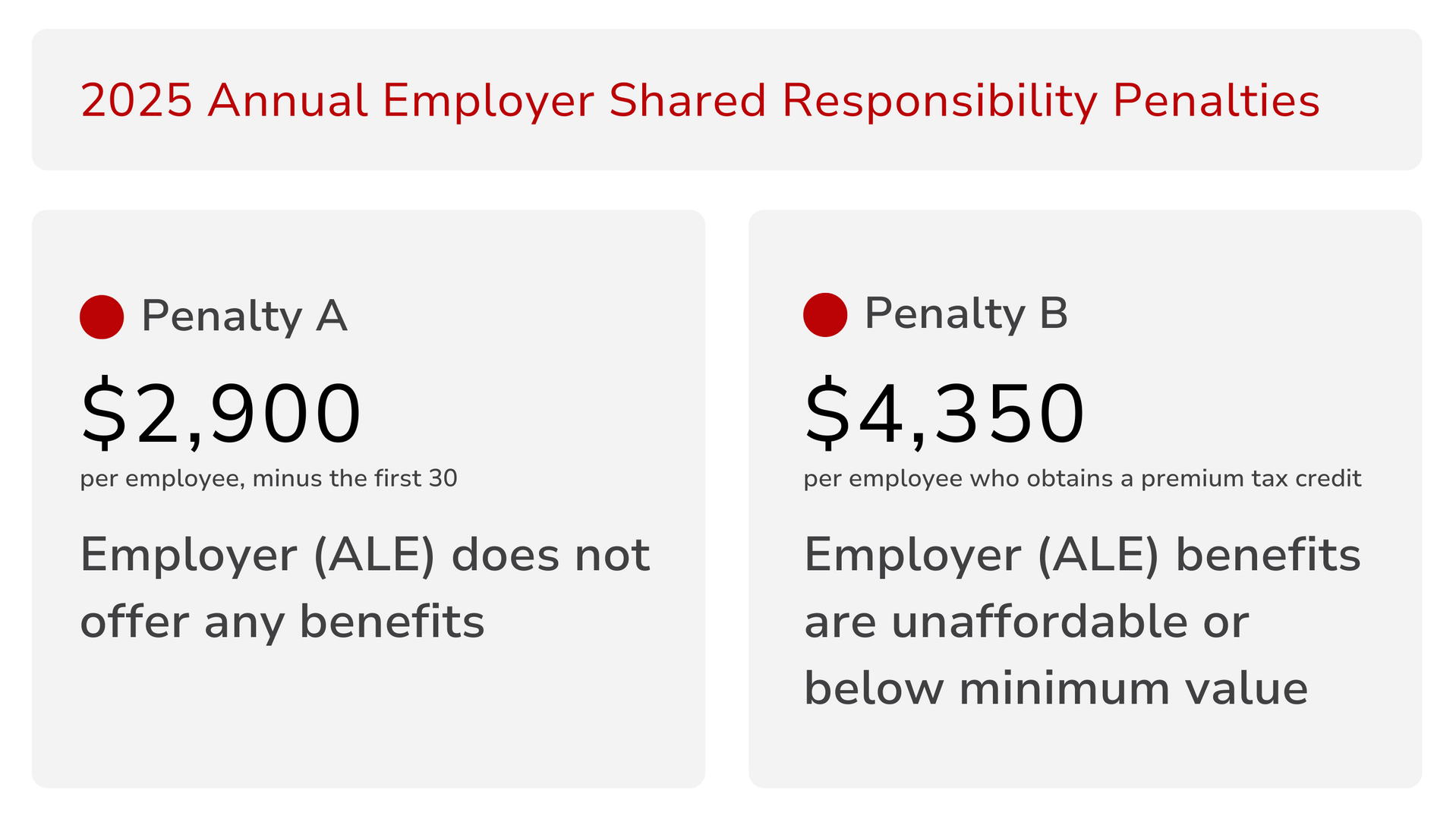
Penalty A: No coverage offered
This penalty is triggered if you offer nothing, or don’t offer coverage to at least 95% of your full-time employees.
Penalty B: Insufficient coverage offered
This penalty is triggered if one of your full-time employees gets a premium tax credit because the coverage you’ve offered is either unaffordable or doesn’t meet the ACA’s minimum value standards.
2025 ACA penalty updates
Employer Shared Responsibility
As stated earlier, the Section 4980H penalty amounts are going down this year. If you are an ALE, this shift represents an opportunity to reassess your healthcare strategy and make sure you’re complying with the law—without unnecessary penalties eating at your bottom line.
- 4980H-A - $2,900 per full-time employee (down from $2,970)
- 4980H-B - $4,350 per full-time employee receiving a tax credit (down from $4,460)
Reporting
While the 4980H penalties have been reduced for this tax year, some of the reporting penalties under sections 6055 and 6056 have increased.
- Failure to report -> $330 per return (up $20)
- Corrections to a filed report
- made within 30 days -> $60
- made after 30 days, but before 8/1/25 -> $130 per return (up $10)
- Intentional disregard -> $660 or 10% of the total reported amount (up $30)
2025 Reporting Deadlines
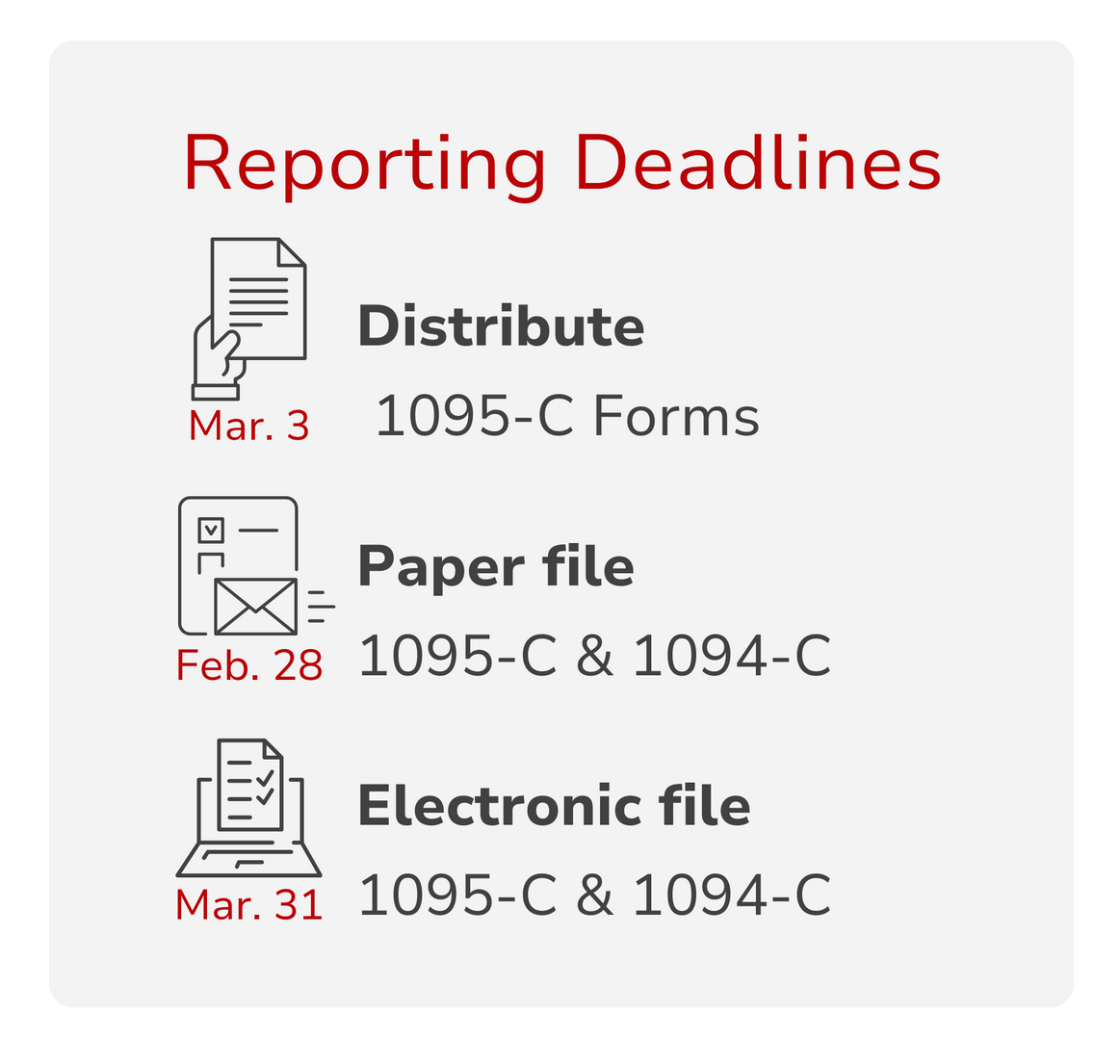
The deadline to provide individual, 1095-C statements to your employees is also unique this year. Typically the deadline is January 31st, but this year, the deadline is March 3, 2025.
Also unique to this year, thanks to new legislation, employers may opt to provide employees with a clear notice that their forms are available upon request, rather than providing each individual with a 1095-C form automatically.
The deadline to file forms 1095 and 1094 with the IRS is February 28 by mail, or March 31 for electronic submission.
Impact on you
Though the penalties are dropping slightly, compliance is still the smartest move—especially since penalties for intentional disregard are going up. For now, it’s critical for you to understand if you are an ALE with a responsibility to report. If you are, you should review your health plan offering and make sure you are meeting the ACAs minimum requirements. This includes evaluating your health plan’s affordability and the extent of plan coverage. Additionally, you will want to verify that you have indeed made offers of coverage to all eligible employees.
- Verify your ALE status
- Review your plan offering
- Confirm you’ve made offers of coverage
- Report to the IRS
We’re here to help you handle the finer points of compliance and navigate the benefits maze without the stress. Whether you need a full compliance checkup or a more cost-effective benefits solution, we’ve got you covered.
For detailed information from the IRS about penalties and deadlines, read this.
To learn more about your responsibilities as an ALE,
read this.
Want to make sure your business is protected from penalties in 2025? Let’s talk.
Give us a call at 888-920-7526 or click the link below to speak with a Benefit Guide.
Explore
SUGGESTED FOR YOU

I WANT TO...
LOGIN
CLAIM INFORMATION
Payer ID: 65241
Planstin Administration
P.O. Box 21747
Eagan, MN 55121
© 2025 Planstin Administration - All Rights Reserved



