The Future of Telehealth and the Impact on Healthcare
Telehealth is changing healthcare. What was once more of a niche service is now becoming a normal part of healthcare—and, for many, the preferred channel for personalized care.

In This Article
Also called telemedicine or virtual care, this type of service really boomed during the COVID-19 pandemic, when more people had exposure to it and discovered how convenient and cost effective this growing form of healthcare can be. To understand how the future of virtual healthcare might shape up, it’s important to understand its appeal, its challenges, and the potential it holds to really change the way we receive care.
The current state of telehealth
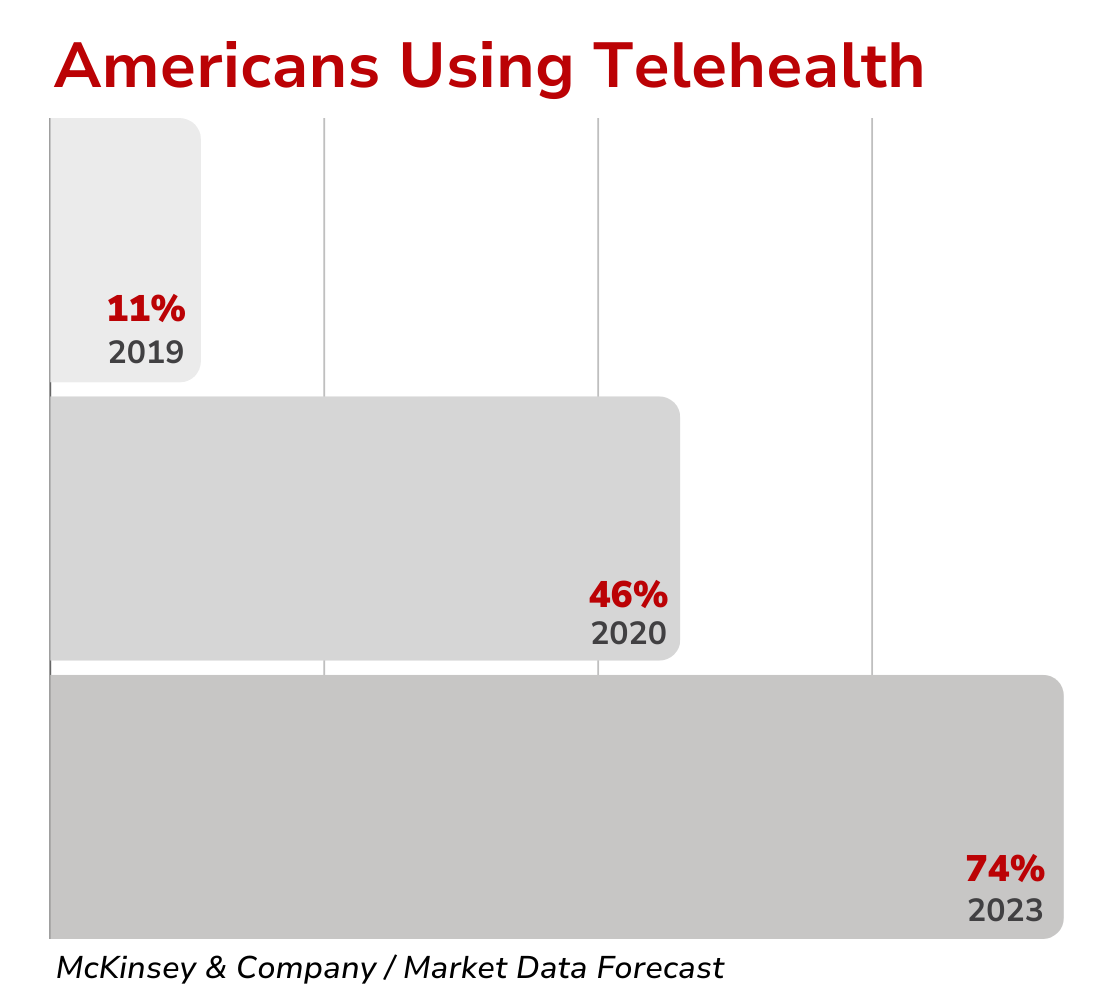
The last several years have seen healthcare finding new forms in the development and adoption of telehealth services, certainly accelerated by the COVID-19 pandemic. Telehealth has shifted from being a new and niche service to what now looks to be a core component of healthcare in the United States. Prior to the pandemic, only 11% of US consumers had used telehealth services, but by mid-2020, this number had jumped to 46%. The constraints of in-person visits at the time introduced many people to this emerging form of healthcare.
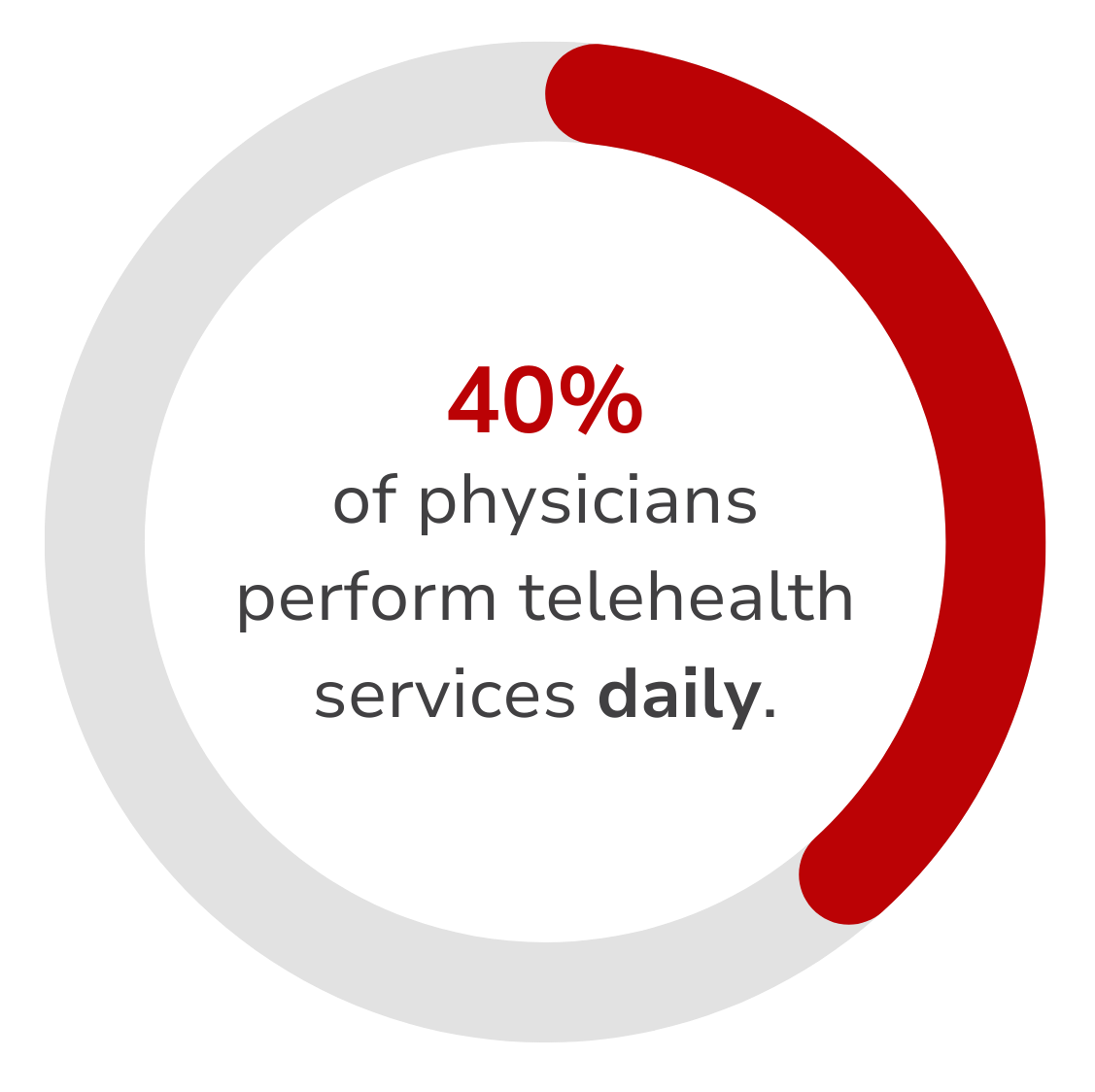
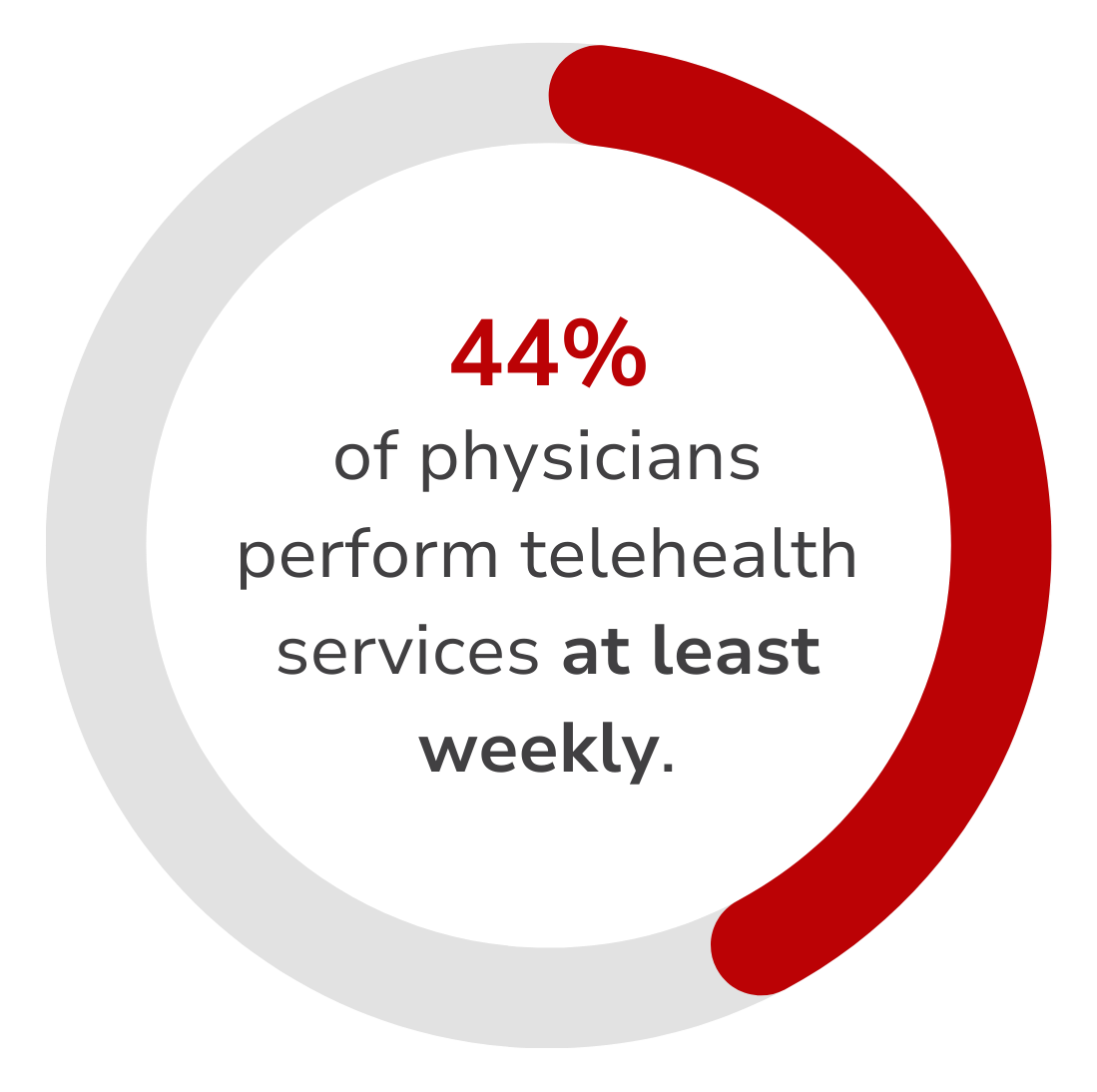
During the peak of the pandemic, more than 97% of healthcare professionals were performing telehealth services, with 43% conducting at least half of their appointments virtually. This has continued, with 44% of US physicians performing telehealth services at least weekly, and 40% of them daily as of 2023, according to a survey by Statista.
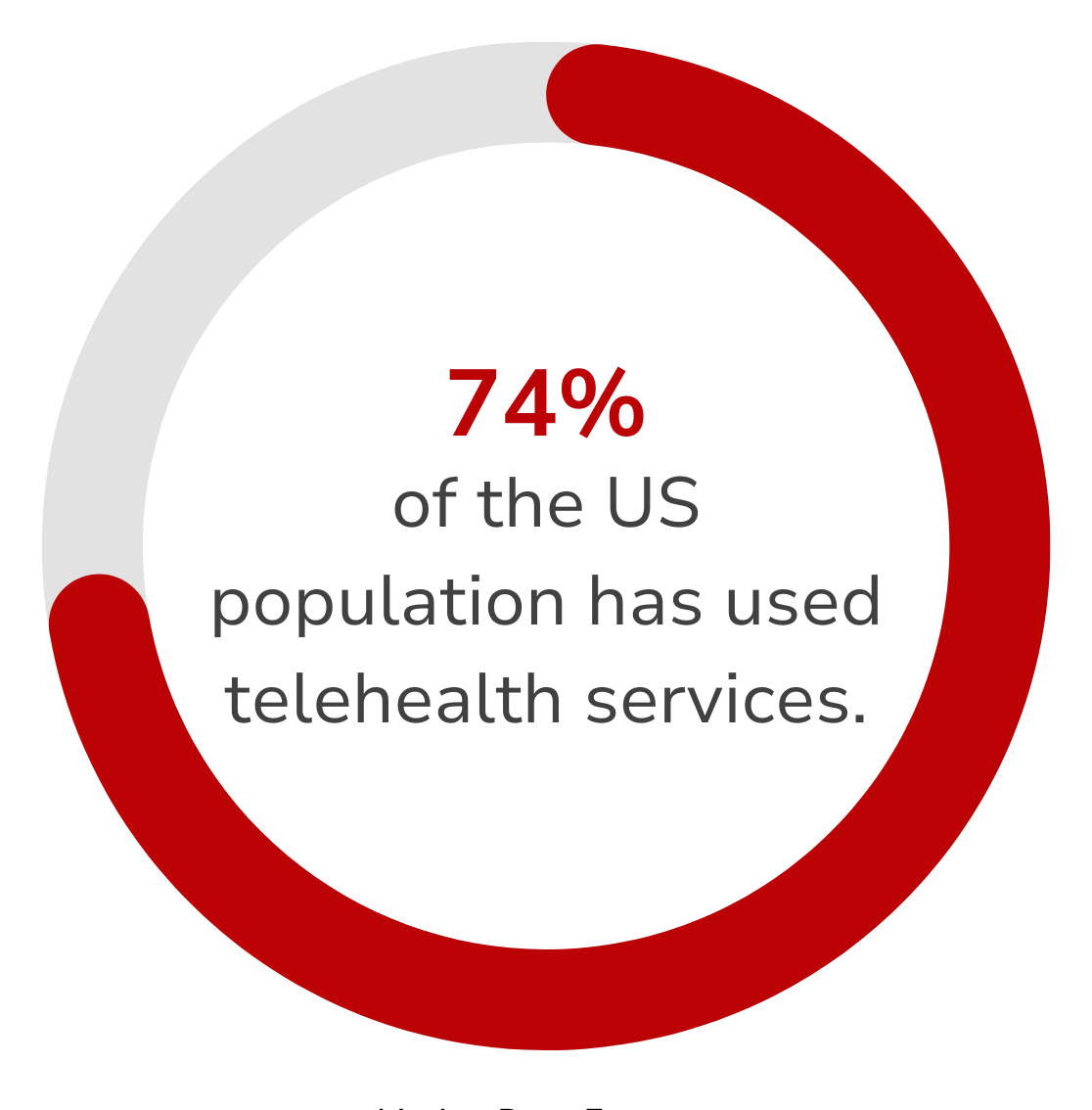
Patient adoption has also been considerable, with approximately 74% of the US population having used telehealth services. This form of healthcare hasn’t just been gaining traction—it’s gained a foothold and become an essential part of healthcare.
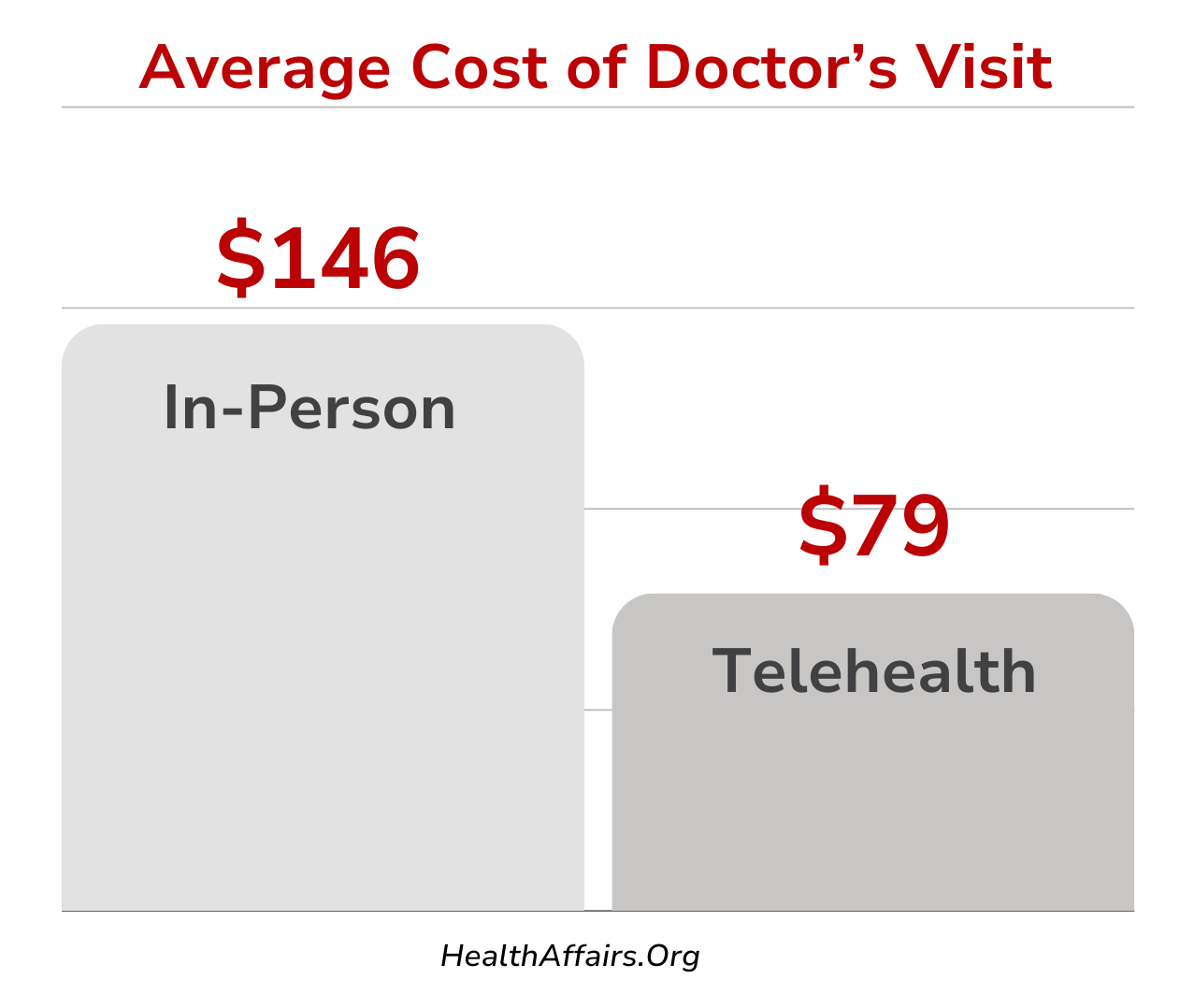
The secret of telehealth’s success
While pandemic-era restrictions may have been the primary driver for the growth of telehealth, there are other explanations for its continued success. One major factor is affordability. On average, a virtual telehealth appointment costs about $79, compared to $146 for an in-person office visit. This cost reduction is even larger when you consider more recent virtual care subscriptions that allow for unlimited visits for a low flat monthly fee. This cost difference makes telehealth an attractive healthcare option for patients and healthcare providers, reducing overall expenses by minimizing the need for physical facilities and allowing for more appointments with more patients.
Another important factor is convenience, largely facilitated by more recent developments in technology. With the widespread presence of smartphones, tablets, and reliable internet connections, patients can now consult with healthcare professionals from their homes, eliminating the need for travel and reducing wait times.
Apps are now available specifically to accommodate telehealth services, allowing it to be more directly integrated into regular healthcare practices.
Impact on patients
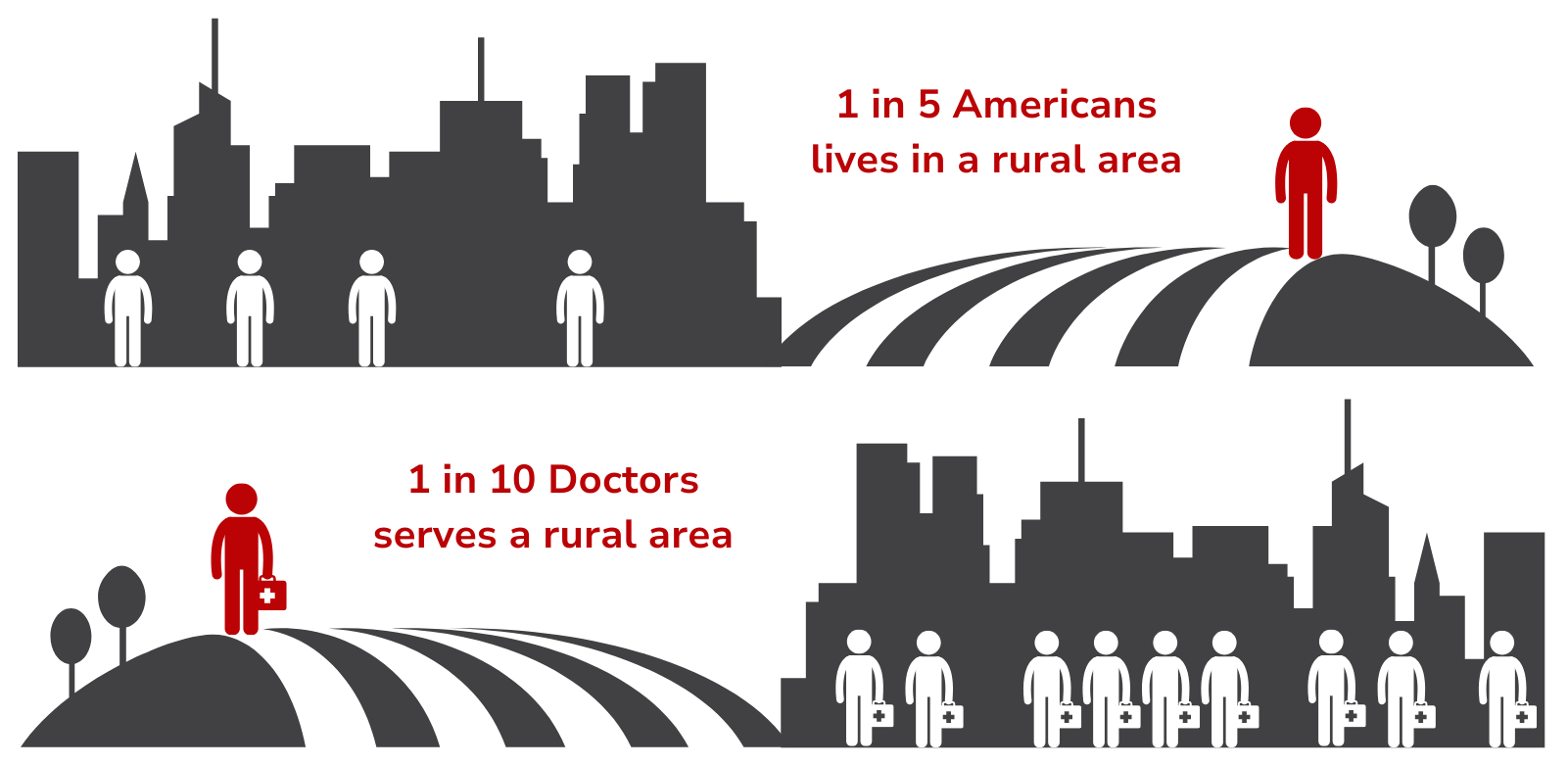
Telehealth has positive effects on patients, particularly in rural areas, by bridging a gap in practical healthcare access. In regions where healthcare providers are few and far between, telehealth services allow patients to consult with specialists and receive timely care without the need for extensive travel.
A 2022 study found that while 20% of the population lives in rural areas, only 9% of physicians serve these same areas. This means that many rural patients simply do not have access to a healthcare provider in their area, or they must be burdened by substantial travel costs in order to see one. This is a where telehealth services are starting to stand out, eliminating the need for travel, while still allowing patients to receive care.
Barriers and drawbacks of telehealth
While telehealth evidently offers numerous benefits, it is not without its challenges, many of which can impact both patients and providers. For virtual care services to be integrated and become a core component of standard healthcare, the issues below will need to be addressed.
Technology and Accessibility
Approximately 21 million Americans lack high-speed internet access, particularly in rural areas. While audio-only consultations are a workaround, they are often insufficient for proper medical attention. Additionally, around 20% of older adults struggle with digital tools, making it difficult for them to use virtual care platforms effectively.
Security and Privacy
Because these services are built on digital systems, security remains a considerable issue, with the healthcare industry seeing a 25% increase in successful cybersecurity attacks during the pandemic. The frequency of these attacks is sure to increase as additional smaller services launch their own platforms, leaving patient information potentially exposed.
Reimbursement Issues
How insurance treats telehealth services is inconsistent, and reimbursement rates often lag behind those for in-person services. This could create financial challenges for providers fully embracing telehealth.
Quality of Care
Some healthcare professionals worry that virtual care may not allow for thorough examinations, potentially leading to more frequent misdiagnoses. Much of the time, attempting to treat illnesses or conditions of a certain nature are harder to address virtually and can, according to Health Affairs, lead to increased spending (though it should be noted that this is telehealth data collected pre-pandemic).
What comes next for telehealth?
Despite the challenges, telemedicine and virtual care are showing no signs of slowing. We should expect this form of healthcare to continue to grow and develop as new technologies emerge and policies enacted.
Healthcare-Centered Software & Business
The development of new software and virtual care platforms is streamlining patient-to-provider communication, improving scheduling, reminders, and overall management of personal healthcare. Practitioners are launching their own independent programs and channels to act as virtual direct primary care providers, building up more close relationships with their patients and fulfilling the needs they perceive in their markets—and typically at a cost savings for the patient.
Integration with Traditional Care
Providers understand that virtual care can serve to complement their in-person visits, creating a flexible model that combines remote and face-to-face interactions. This allows initial consultations and follow-ups to be conducted online, while reserving in-person visit times for more complex cases. For example, patients can manage chronic conditions through regular virtual check-ins and only visit their provider in person for necessary tests or physical examinations.
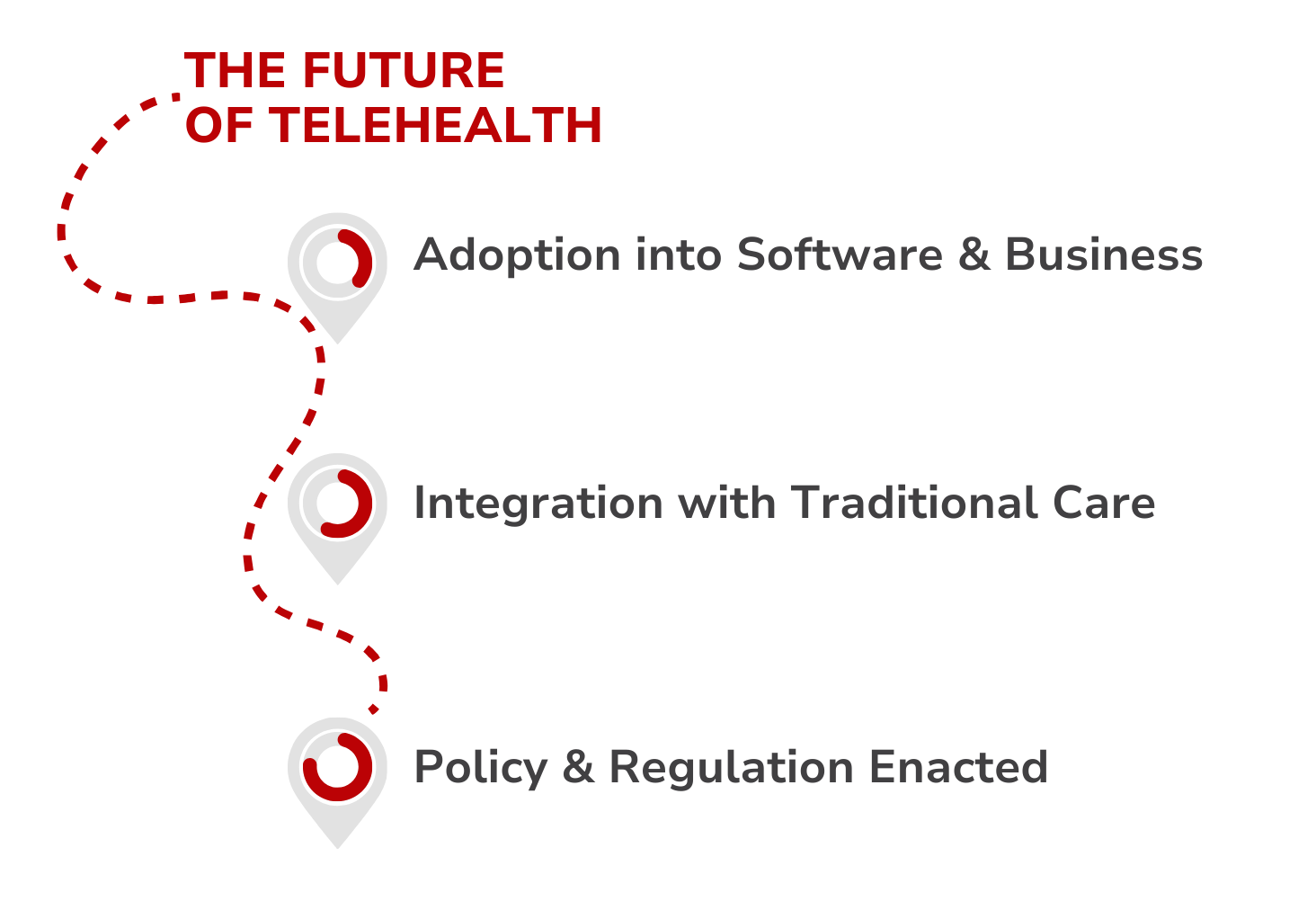
Policy and Regulation
The rise of telemedicine and virtual care has happened fast, and policymakers are still trying to catch up. Efforts are underway, led by the American Medical Association, to reach price parity so that insurance companies will cover telehealth services as they would traditional in-person visits. During the COVID-19 pandemic, temporary regulatory changes expanded telehealth coverage and access. Now that the benefits of telehealth are more widely understood, policymakers areconsidering making some of these changes permanent. Policy support like this will only help the continued growth of telemedicine and its integration into the wider healthcare system. Expanded coverage and increased reimbursement rates for telehealth services will be important for sustaining its growth.
Telehealth is modern healthcare
Healthcare has changed substantially from what it looked like just a few years ago, and telehealth and virtual care are a large part of that change. While there are certainly challenges to overcome, its affordability, convenience, and its ability to broaden healthcare access are hard to overlook.
With ongoing technological improvements and supportive policy changes, telehealth is positioned to become a core part of our healthcare system.
Offering telehealth benefits is within reach. Book a free meeting with one of our Benefit Guides to learn how you can make virtual care available to your team.
Explore
SUGGESTED FOR YOU

I WANT TO...
LOGIN
CLAIM INFORMATION
Payer ID: 65241
Planstin Administration
P.O. Box 21747
Eagan, MN 55121
© 2025 Planstin Administration - All Rights Reserved